Understanding CAR-T cell therapy: The Living Drug
In the rapidly evolving field of oncology, few breakthroughs have generated as much excitement and hope as Chimeric Antigen Receptor (CAR) T cell therapy—an innovative treatment often dubbed a “living drug.” This cutting-edge immunotherapy is not just a new class of treatment; it represents a fundamental shift in how we think about fighting cancer—by empowering the body's own immune system to destroy malignant cells.
While the science behind it is complex, this guide aims to explain CAR-T cell therapy in a way that is clear and accessible to the general public.
What is CAR T Cell Therapy?
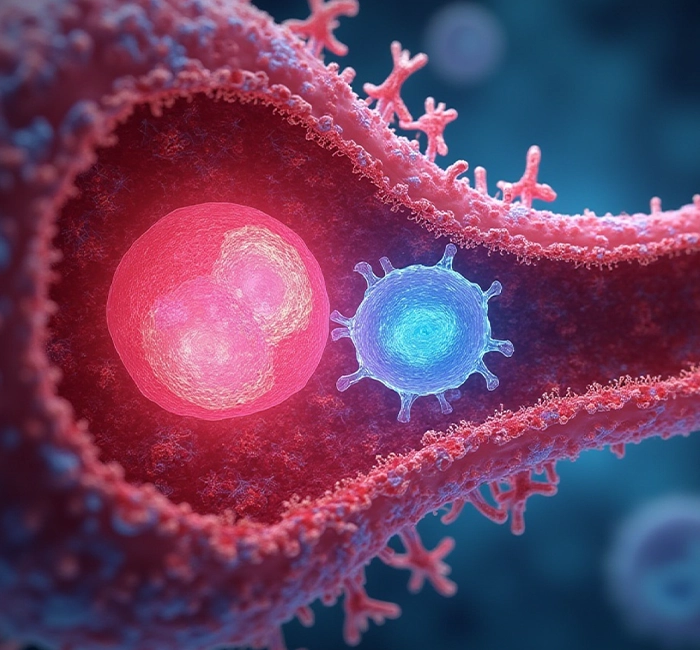
CAR T cell therapy is a type of immunotherapy — a treatment that uses the immune system to fight diseases like cancer. “CAR” stands for Chimeric Antigen Receptor, a specially designed receptor that is added to a patient's T cells. T cells are a type of white blood cell that normally helps the body fight infections.
With CAR T cell therapy, doctors take a patient's own T cells, reprogram them in a lab to recognize cancer cells, and then put them back into the patient's body. Once inside, these modified T cells can find and kill cancer cells with precision.
How Does the Treatment Work?
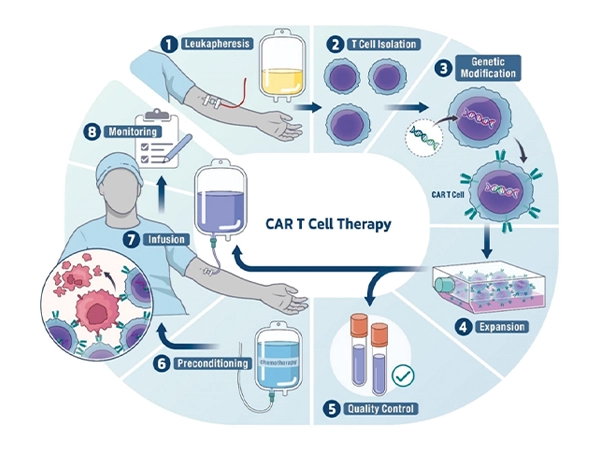
The treatment process usually involves several steps:
-
Collecting T Cells: Blood is taken from the patient, and T cells are separated out. Engineering the T Cells: In a lab, the T cells are genetically modified to produce CARs (chimeric antigen receptors). These new receptors help the T cells recognize cancer cells more easily. Multiplying the T Cells: The modified cells are grown and multiplied until there are millions of them.
-
Infusing the Cells: The patient is given a short course of chemotherapy to weaken their existing immune system, then the engineered T cells are infused back into the bloodstream. Fighting Cancer: Once in the body, the CAR T cells seek out and destroy cancer cells
What Types of Cancer Can CAR T Treat?
Currently, CAR T cell therapy has been approved for certain types of blood cancers, including:
What Are the Benefits?
Targeted Attack
CAR T cells are specifically trained to recognize cancer cells, minimizingdamage to healthy cells.
Long-Lasting Effects
In some patients, CAR T cells remain in the body and continue to guard against cancer returning
Hope for the Hard-to-Treat
It offers hope to patients who have not responded to traditional treatments like chemotherapy or radiation.
Process Flow
If needed, a certified treatment centre will help start the enrolmentprocess. The doctor will then check if the patient is suitable for CAR-T cell therapy
Seven Steps in CAR T-cell Therapy
Screening and Registration
Apheresis
CAR T-cell Manufacturing
Lymphodepletion Preparative Regimen
Hospitalization and CAR T-cell Infusion
Post-Infusion Monitoring
Follow-up
Are There Any Risks or Side Effects?
Like many powerful treatments, CAR T therapy is not without risks. Common side effects include:
- Cytokine Release Syndrome (CRS): A strong immune response that can cause fever, low blood pressure, and difficulty breathing
- Neurological Symptoms: Confusion, tremors, or seizures can occur in some patients.
- Infections: Because the immune system is affected, patients may be more vulnerable to infections.
Doctors monitor patients closely and have treatments ready to managethese side effects if they occur.

Is CAR T Therapy Available Everywhere?
CAR T-cell therapy is available only at selected advanced cancer centers in India with expertise in cell and gene therapy. Medical Trust Hospital, Kochi, is a pioneering center in South India, distinguished for its successful implementation of this innovative treatment. Our state-of-theart CAR-T cell therapy unit is dedicated to delivering cutting-edge cellular therapy
What Does the Future Hold?
CAR T cell therapy is a shining example of personalized medicine — a treatment tailored to a patient's own body. As research continues, scientists hope to improve its safety, expand its use to more cancers, and even combine it with other therapies for better results.
Glossary
- Antigen: A marker on cells that helps your immune system identify normal cells from infected or cancerous cells
- B-cells: Along with other cells, they make up your body immune system.They defend the body by producing antibodies.
- CAR T-cell therapy: A specific type of cancer treatment. The CAR in CAR-T stands for chimeric antigen receptor, and the T stands for T-cell
- CD19: An antigen located on your B-cells
- Chimeric: Having parts of different origins
- CRS (Cytokine Release Syndrome): A side effect that can happen when the immune system is highly activated
- Immunotherapy: A type of cancer treatment that helps your immune system fight cancer
- Leukapheresis: When your doctor takes some of your blood to collect your T-cells
- Refractory: Your cancer did not respond to treatment
- Relapsed: Your cancer has returned
- Remission: The signs of your cancer have disappeared, or else your disease is under control. It does not necessarily mean a cure
- T-cells:Along with other cells, they make up your body's immune system. They are natural defenders that detect and destroy possible threats such as infected or cancerous cells
Frequently Asked Questions
Getting to Know CAR T-cell Therapy
- Is CAR T-cell therapy the right treatment for you?
- Take a closer look at the treatment journey
- Can CAR T-cell therapy work for me?
- What do doctors check before starting it?
- If not now, could it be an option later?
- What proof is there that it works?
- What happens during my hospital stay?
- What to expect before CAR-T therapy
- Can CAR T-cell therapy work for me?
- What do doctors check before starting it?
- If not now, could it be an option later?
- What proof is there that it works?
- What happens during my hospital stay?
- What happens during the infusion
- Can CAR T-cell therapy work for me?
- What do doctors check before starting it?
- If not now, could it be an option later?
- What proof is there that it works?
- What happens during my hospital stay?
- After your CAR T-cell treatment
- Can CAR T-cell therapy work for me?
- What do doctors check before starting it?
- If not now, could it be an option later?
- What proof is there that it works?
- What happens during my hospital stay?

